Over 100 years ago the German psychiatrist Alois Alzheimer published his post-mortem neuropathological observations in former patient Auguste Deter, who had exhibited a complete degeneration of the psyche in the years before her death, and whose brain showed the now-classic hallmarks of senile plaques and neurofibrillary tangles in the disease that now bears his name. 100 years later, Alzheimer’s disease (AD) is an ever-growing public health problem with over 1 million cases expected in the UK by 2025; the clinical effects of cognitive decline and dementia (of which AD is the most common cause) remain as devastating as ever.
Much of the research into the origins and treatments for AD has focused on the ‘Amyloid Cascade Hypothesis’ that places the toxic brain proteins of Amyloid-beta and Tau as the primary disease-causing catalysts. Despite this, with the U.S. NIH spending $1.9 billion on research in 2018 alone, our understanding of AD has not progressed much further; the failure rate of AD drug clinical trials currently stands at 99%.
As a result, scientists have begun to think ‘outside the box’ to consider the multifaceted origins of AD, and the multiple peripheral health conditions (such as diabetes and gum disease) that could increase the risk of patients developing the condition. Significant research has also focused on the causes and prevention of neuroinflammation, a local immune reaction and a frequent clinical observation in dementia-afflicted brains.
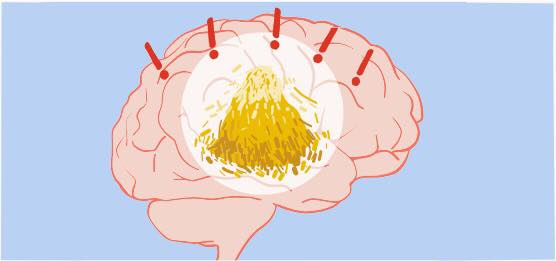
From epidemiological studies in older populations, it was observed that people who had lost teeth as a result of gum disease earlier in life were more likely to develop AD. This was theorised (through research with contributions from Southampton academics) to be from molecules called cytokines being released into the general blood circulation as a result of periodontal (gum) inflammation, when dental plaque is not sufficiently removed during brushing. Cytokines could then migrate to the brain and activate the resident microglia cells into an immune-inflammatory response that exacerbates the neuro-pathology of AD, leading to brain death and dementia
A landmark 2019 study into the role of periodontitis in AD additionally focused on the oral bacteria Porphyromonas gingivalis, and how it acts in conjunction with neuroinflammation to cause AD. Oral infection in mice with this ‘keystone pathogen’ directly led to the formation of senile plaques and neurodegeneration. Furthermore, a small-molecule inhibitor targeting the pathogenic enzymes in Pg reduced the bacterial load, blocked plaque production, reduced neuroinflammation, and rescued hippocampal neurons that would otherwise have been afflicted in dementia.
These results have significant implications for gum disease as an environmentally-modifiable risk factor for AD; further research will focus on how exactly transient bacteraemia (bacterial migration) of P. gingivalis occurs from gums to brain to exert neuro-toxicity. Early interventions aimed at preventing AD through regular dental checkups and oral hygiene education in the general population may thus prove to be extremely effective in reducing the future incidence of dementia.